EMR ROI Calculator for Therapy Clinics
Model your monthly value from admin hours saved, fewer denials, and avoided per-claim fees—then compare to subscription cost for payback.
What drives EMR ROI for PT/OT/SLP
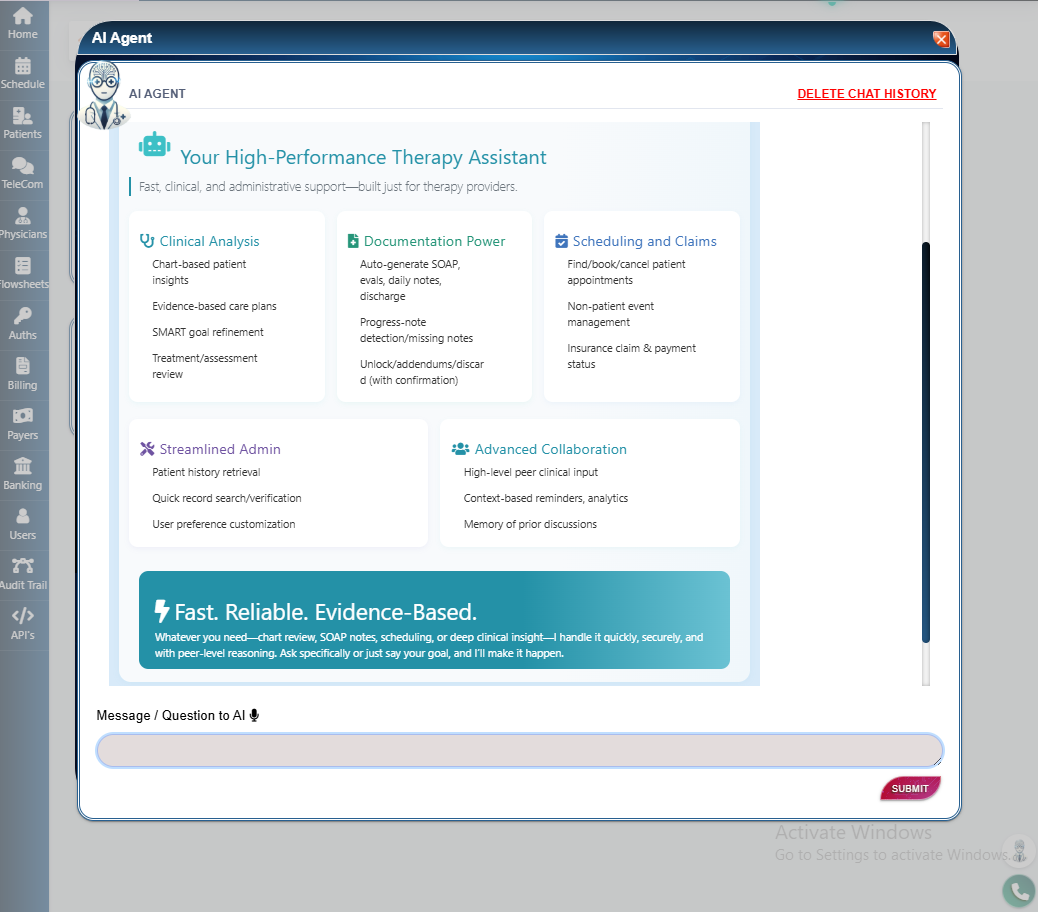
- Less clerical time: Streamlined documentation, eligibility, routing, and auto-posting return hours to care and capacity.
- Fewer preventable denials: A scrubber that flags coding conflicts, missing auth, and common errors before submission reduces rework and keeps A/R clean.
- Avoided tolls and delays: Where available, direct-to-payer connections help clinics avoid per-claim pass-through fees and extra hops.
- Eligibility ≠ payment: Benefits screens are helpful but not a guarantee; confirm details with the payer when in doubt.
Education only; not billing, legal, or financial advice. Your results will vary by payer mix, panel policies, and clinic workflows.
ROI Calculator
Assumptions & simple math
Admin time value = Providers × Hours saved per week × Loaded hourly wage × 4.33 weeks/month.
Fees avoided = Monthly claims × Per-claim fee.
Prevented denials value = Monthly claims × Initial denial rate × Preventable share × Average value per prevented denial.
FAQ
Does eligibility verification guarantee payment?
No. Payers routinely note that eligibility/benefits information is not a guarantee of payment; final payment depends on the plan, member status, and the submitted claim. When in doubt, call the payer’s provider line.
What should I use for my denial rate?
Use your own baseline. If you don’t have one yet, start with a conservative single-digit estimate and refine from remittance data.
Where do time savings come from?
In practice, clinics report fewer clicks and less duplicative work when documentation, eligibility, routing, and ERA posting are integrated. Reducing that load returns hours to patient care and throughput.
How do I compare to cost?
Take the calculator’s monthly value and compare it to your subscription cost. Also include any per-claim or mailed-statement fees you avoid with PBS EMR.