Daily note
4:12
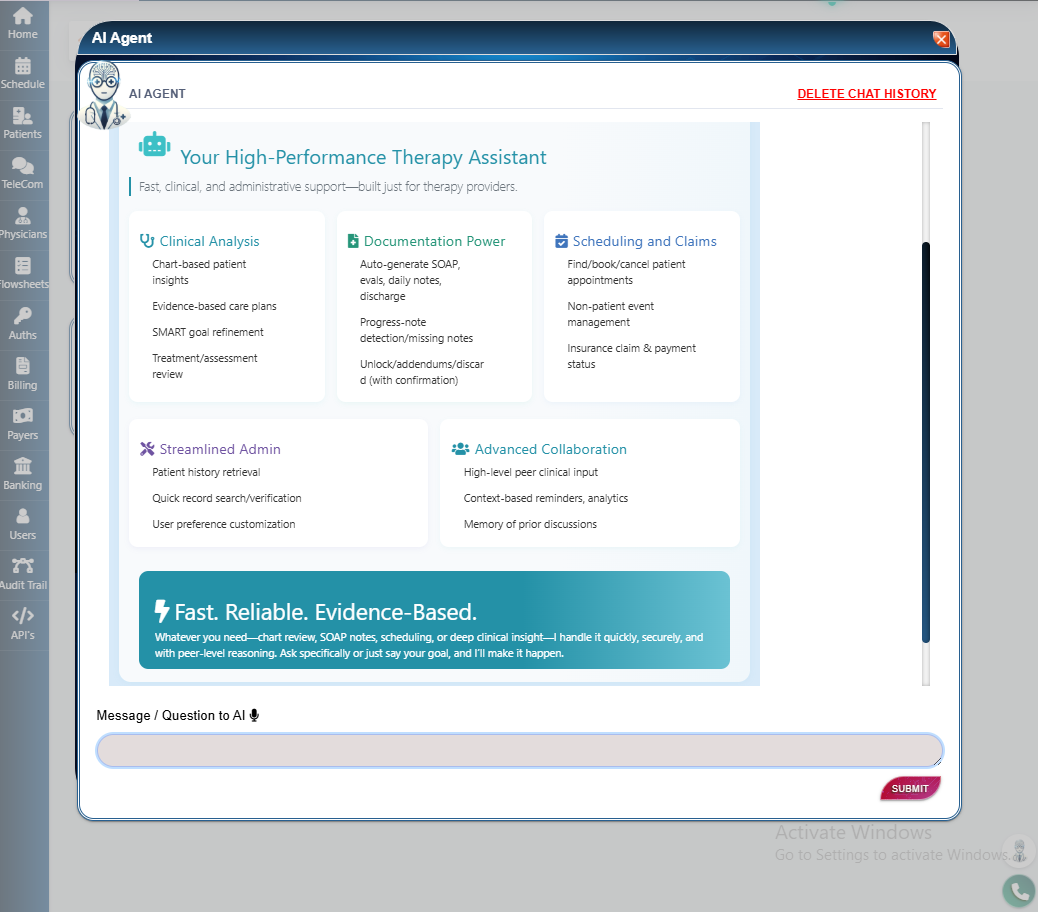
Turn documentation into a clear, clinical conversation. The chart‑native AI co‑pilot stays optional, cites the chart context, and helps you finish fast, defensible notes—so teams spend more time with patients and less on screens.
4:12
6:45
11:30
Medians vary by discipline, payer mix, case complexity, and staffing. Use the ROI calculator with your own numbers.
Interventions and outcomes live together, so progress is defensible and plateaus surface quickly:
When notes finalize, flowsheets and HEP update automatically; suggested codes appear for review—no double entry.
Education only; not legal, medical, or billing advice. Your workflows and payer policies determine final documentation and coding.
Medians reflect timed sessions across pilot outpatient therapy clinics using PBS EMR. Tasks included standard daily, progress, and evaluation notes with typical payer mixes. Times exclude long pauses and administrative interruptions. We refresh medians periodically to reflect real‑world use.
Want to review the approach for your clinic? Email us and we’ll share the timing protocol and help you run a quick on‑site sample.
No. The ambient scribe and all suggestions are optional. You can turn features off or use quick phrases and templates without AI.
Yes. Templates and flowsheets adapt by discipline, domain, and precautions; drafts cite chart context so complex care stays clear.
No. Eligibility and benefits screens help, but payment depends on the claim and plan terms. Follow payer rules and clinic policy.
Delegation‑ready steps with inclusion cues and stop criteria keep tasks consistent and reproducible across teams and locations.